Rheumatoid Arthritis
How is it diagnosed ?
There is No single test.
Instead your physician must look at your entire history, physical examination , laboratory tests and radiographs when making the diagnosis of rheumatoid arthritis. The first step your doctor will take a complete medical history from you. Your age is an important factor when considering the diagnosis. Because most people who develop rheumatoid arthritis are between the age of 20 and 60, if you fall outside of this age range it makes the diagnosis less likely. Common symptoms from rheumatoid arthritis include morning stiffness that lasts for longer than one hour, bilateral symmetrical involvement of small joints (eg. both hands), and multiple joints being involved (often 3 or more).The most common joints to be involved are the fingers , hands, wrists, and feet. Often, people with rheumatoid arthritis may also complain of general fatigue, weakness , low-grade fever without and obvious source of infection, decreased appetite, weight loss, and/or muscle pain. People with rheumatoid arthritis typically will complain of difficulty performing tasks of daily living such as writing, preparing food, grasping a cup, getting dressed, and turning a doorknob. Occasionally, rheumatoid arthritis can affect the heart (pericarditis) in which case the person may have chest pain that is worse when taking a deep breath or when lying down. Almost any organ in the body can become affected by rheumatoid arthritis. When the blood vessels themselves are involved, a vasculitis develops that can be debilitating and dangerous. These complications are more common with long-standing chronic rheumatoid arthritis.
Patients with rheumatoid arthritis will typically not have pain or swelling in the finger joint closest to the fingertip (the distal interphalangeal joint). The other joints in the hand are often affected. The affected joints are often tender to the touch. Depending on how long the person has been having symptoms, and the severity of the rheumatoid arthritis, there may also be some deformity in the fingers, hands, wrists, and other joints. Rheumatoid nodules may develop and be felt as firm lumps beneath the skin. These occur most commonly at points of pressure under the elbow and on the fingers. Usually rheumatoid nodules do not cause pain but they can become infected or put pressure on a nerve in which case they would need to be treated.

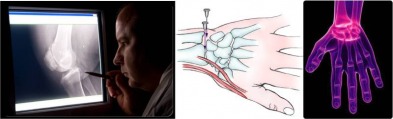
Your doctor will likely order several tests. Blood tests will reveal an anemia (decreased hemoglobin) in 80% of patients with rheumatoid arthritis. The erythrocyte sedimentation rate (ESR) is a general marker of inflammation and is elevated in 90% of patients. In 70% of rheumatoid arthritis a marker called rheumatoid factor (RF) will be present. However, all of these tests are nonspecific and may be positive in people without rheumatoid arthritis. The results of these tests need to be integrated by your physician with your other findings to make the diagnosis of rheumatoid arthritis.
On radiographs (x-ray), the typical findings of rheumatoid arthritis include cysts, osteopenia, swelling, bony erosions, narrowed joint space, deformities, and fractures. Your physician may perform an arthrocentesis of the affected joint or joints. This procedure involves putting a needle under sterile conditions into the affected joint and aspirating the fluid. The fluid is then sent for analysis. This procedure is used in this setting to rule out other possible etiologies of the pain and swelling such as infection, gout, and pseudogout. In a person with suspected rheumatoid arthritis and neck pain or neurologic symptoms (pain, numbness, weakness radiating into the arms or legs), the physician should perform tests to ensure that there is no instability of the cervical spine (vertebrae in the neck) because people with rheumatoid arthritis are more susceptible to this type of instability than the general population.
Courtesy: Arthritis Organisation
Courtesy: Arthritis Organisation